How to deliver oxygen to a NYI
Learning objectives
After completion of this session the participant should be able to:
- Describe when oxygen is needed
- Know how to deliver oxygen therapy
- Know when to stop oxygen therapy
An infant who has signs of severe respiratory distress requires oxygen
- Grunting
- Cyanosis
- Head nodding
- Respiratory rate >80/min
- Severe lower chest in-drawing
- Apnoeic spells
- Unable to feed due to respiratory distress
Confirm with oxygen saturations if available -> The NYI requires oxygen if oxygen saturation is less than 90% (<90%)
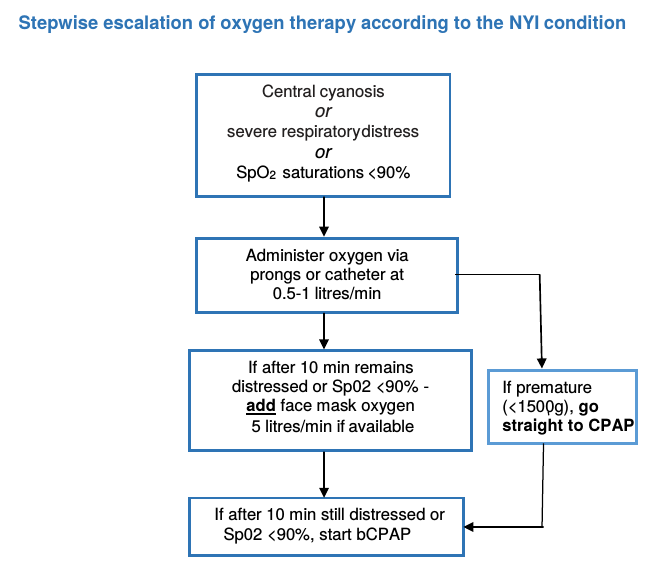
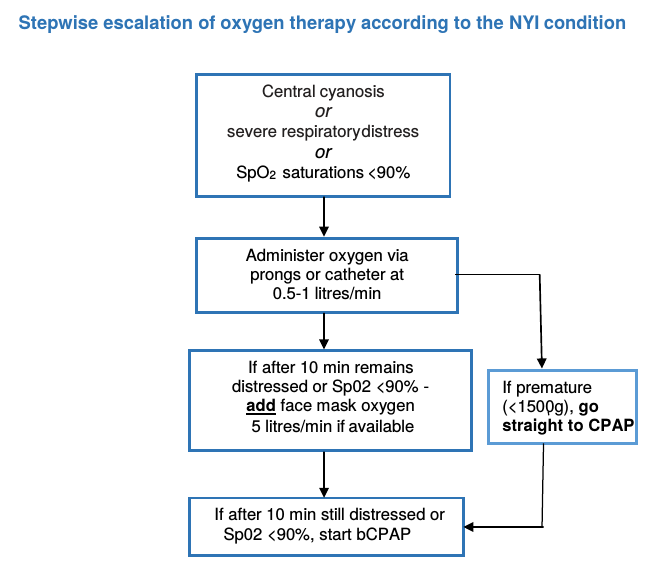
A baby with cyanosis or severe respiratory distress should be allowed to take a comfortable position of his choice and should be given oxygen immediately via prongs or catheter. Escalate the oxygen therapy in a stepwise fashion depending on availability.
If the baby’s breathing difficulty does not improve on prongs or catheter oxygen, despite increasing the flow:
Place the NYI on oxygen at a high flow rate (5 litres/min) via face mask if possible or if this is unavailable, or if the breathing difficulties persist then place the baby on bCPAP if available
Monitor and teach the mother to monitor the infant, look for the following problems
1. Displacement of the prongs or catheter
2. The concentrator malfunctioning or being accidentally switched off
3. The airways may become blocked with mucus
4. The abdomen may become distended with air
5. Increased respiratory distress
If breathing difficulty is so severe that the baby has central cyanosis even with high flow oxygen or bCPAP, rule out a pneumothorax with a chest x-ray if available. Discuss with senior colleague.
When and how to stop oxygen therapy
Continue giving oxygen until the infant is able to maintain a SaO2 >90% in room air. When stable and improving, take the infant off oxygen and recheck oxygen saturations after 30 minutes. If the infant’s saturations remain above 90% s/he may remain off oxygen but check the saturations 4-hourly thereafter on the first day off oxygen to ensure the child is stable.
Where pulse oxymetry is not available, the duration of oxygen therapy is guided by clinical signs. If oxygen saturations are not available the oxygen can be stopped if the baby does not have respiratory distress, but keep under review and recommence if the respiratory distress increases after stopping the oxygen.
Avoid prolonged SpO2 >95% in premature newborn infants.
Sources and delivery methods of oxygen
Oxygen concentrator: The source of oxygen is generally the oxygen concentrator. These usually deliver 5 -10 litres of oxygen per minute and there is a gauge for adjusting the concentration of oxygen. The filter at the back of the concentrator should be cleaned every week to keep them working well. Sufficient oxygen should be given to keep oxygen saturations above 90%.

Nasal Prongs: Prongs come in different sizes. Nasal prongs are preferred over nasal tube or catheter for delivering oxygen to young infants. Place them just inside the nostrils and secure with a piece of tape on the cheeks near the nose. Take care that the nostrils are kept clear of mucus, which could block the flow of oxygen. A flow rate of 0.5-1 litres/min will deliver 30-35% oxygen concentration in the inspired air. Aim for oxygen saturations >90%.

Nasal tube or catheter: Use 8 French size catheter. Determine the distance the tube should be passed by measuring the distance from the side of the nostril to the inner margin of the eyebrow. Gently insert the catheter into the nostril. A flow rate of 0.5-1 litres/min in infants will deliver 30-35% oxygen. Aim for oxygen saturations >90%.

A simple face mask will deliver 40-60% oxygen in an emergency and if the infant is very distressed. A minimum of 5 litres of oxygen per minute is needed to prevent rebreathing of expired air. A face mask with a reservoir attached will deliver 100% oxygen. It may be used for resuscitation. The problem with this method is that it may require one concentrator per NYI, which may be challenging if several NYIs require oxygen at the same time. Aim for oxygen saturations >90%.